Hodgkin’s lymphoma (HL) is one of oncology’s greatest success stories, with high cure rates and long-term survival—especially in early-stage disease. However, this success has uncovered an important reality: in patients with early Hodgkin’s lymphoma, cardiovascular disease becomes the leading cause of death in the long term, surpassing cancer-related mortality. Understanding and mitigating this risk is now a critical part of survivorship care.
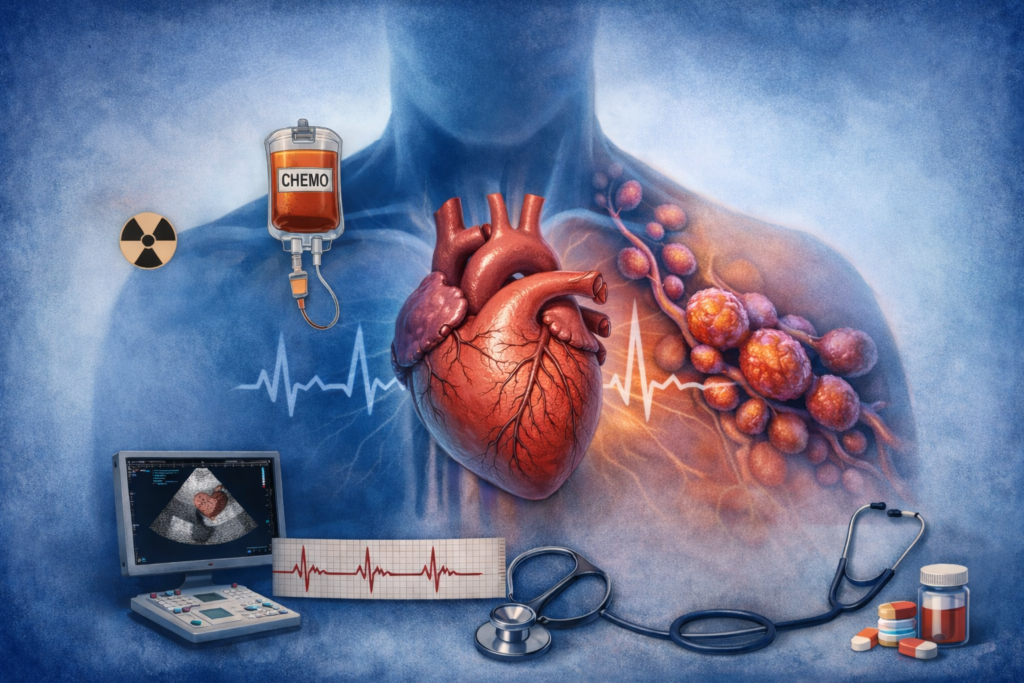
Two major contributors drive cardiovascular complications in HL survivors: anthracycline chemotherapy and radiation therapy. Historically, radiation was routinely used in early-stage disease. Over time, data demonstrated that its long-term cardiovascular risks often outweighed its benefits, leading to its omission in most modern early-stage treatment protocols. Despite this shift, many survivors treated years or decades ago were exposed to mediastinal radiation and remain at elevated risk today.
Anthracyclines, a cornerstone of HL therapy, carry well-established cardiotoxic potential that is dose dependent and cumulative. Efforts to reduce total anthracycline exposure have helped lower risk, but cardiotoxicity remains a concern. The likelihood of cardiac complications increases with higher cumulative doses, older age at treatment, and the presence of traditional cardiovascular risk factors such as hypertension and diabetes. The concurrent use of other cardiotoxic therapies and prior radiation further amplifies this risk. Clinically, anthracyclines most commonly lead to heart failure, while arrhythmias occur less frequently.
For survivors who previously received radiation therapy, the spectrum of cardiovascular disease is broader and often delayed. Radiation induces oxidative stress, endothelial injury, fibrosis, and chronic inflammation, setting the stage for accelerated cardiovascular aging. This can manifest as premature coronary artery disease, valvular heart disease, restrictive cardiomyopathy, pericardial thickening, and scar-related arrhythmias—usually noted decades after cancer treatment has ended.
Given this complexity, risk-based cardiovascular surveillance is essential. Monitoring strategies are tailored according to an individual’s cumulative exposure and risk profile. Transthoracic echocardiography remains a cornerstone for assessing cardiac structure and function, while biomarkers such as troponin and NT-proBNP may be used before, during, and after chemotherapy to detect early myocardial injury or strain. Long-term survivors often require ongoing surveillance even when asymptomatic.
Currently, evidence supporting routine use of medications for primary prevention of cardiotoxicity is limited. However, once cardiovascular disease or dysfunction is identified, guideline-directed medical therapy should be promptly initiated. Equally important is aggressive management of modifiable risk factors, including hypertension, diabetes, and dyslipidemia.
Perhaps the most powerful—and underutilized—intervention is lifestyle optimization. Regular physical activity, heart-healthy nutrition, weight control, adequate sleep, and stress management play a central role in reducing long-term cardiovascular risk. For Hodgkin’s lymphoma survivors, survivorship does not end with remission; it evolves into proactive cardiovascular care.
Early recognition, individualized monitoring, and a strong emphasis on prevention allow survivors not only to live longer—but to live well.
— Anusha Bhat, MD, MPH
Cardio-Oncology | Cardiovascular Disease
Cardio-oncology educational site
