
Why Dyslipidemia and Cardiovascular Comorbidities Cannot Be Ignored
A cancer diagnosis changes everything.
What it should not change is how we manage cardiovascular risk.
The average patient is diagnosed with cancer in their early 60s—an age at which cardiovascular disease is already common. By the time cancer enters the picture, many patients are living with at least one established cardiovascular risk factor: hypertension, diabetes, obesity, or dyslipidemia. These conditions do not pause during cancer treatment. Instead, they often fade into the background—overshadowed by the urgency of cancer care—creating a silent but growing threat.
When Preventive Care Quietly Disappears
Evidence shows that adherence to cardiovascular medications declines substantially after a cancer diagnosis. In a large cohort of patients with breast cancer, adherence to statin therapy dropped by nearly one-third by two years after diagnosis compared with the year prior. By three years post-diagnosis, only half of patients remained compliant with statin therapy—even among those who never received systemic chemotherapy (1).
This pattern is not isolated to statins. Similar declines in adherence have been observed with medications for hypertension and diabetes, underscoring a broader problem: once cancer treatment begins, chronic cardiovascular disease management often becomes collateral damage (2).
The result is predictable—and preventable. Cardiovascular risk accumulates silently while attention is focused elsewhere.
Dyslipidemia: Common, Underappreciated, and Biologically Relevant
Abnormal lipid profiles are present in nearly one in two patients with cancer, with particularly high prevalence in breast and prostate cancer populations. Dyslipidemia in cancer is not merely incidental; it is intertwined with cancer biology itself.
Cancer cells undergo metabolic reprogramming to sustain rapid growth. This includes increased cholesterol synthesis and uptake, coupled with reduced cholesterol efflux, allowing intracellular cholesterol accumulation to meet heightened metabolic demands. In simple terms: cancer cells hoard cholesterol to survive and multiply.
This biological link has sparked interest in statins as potential anticancer agents. However, studies examining statin use and cancer incidence or cancer-specific mortality have largely yielded neutral or negative results. These findings have, at times, fueled hesitation among patients and providers regarding statin continuation during cancer therapy.
But this misses the point.
The purpose of statin therapy is not to treat cancer—it is to prevent cardiovascular morbidity and mortality. Abandoning statins during cancer treatment does not protect patients; it exposes them to avoidable cardiovascular harm.
Cancer Therapy, Physical Inactivity, and Metabolic Decline
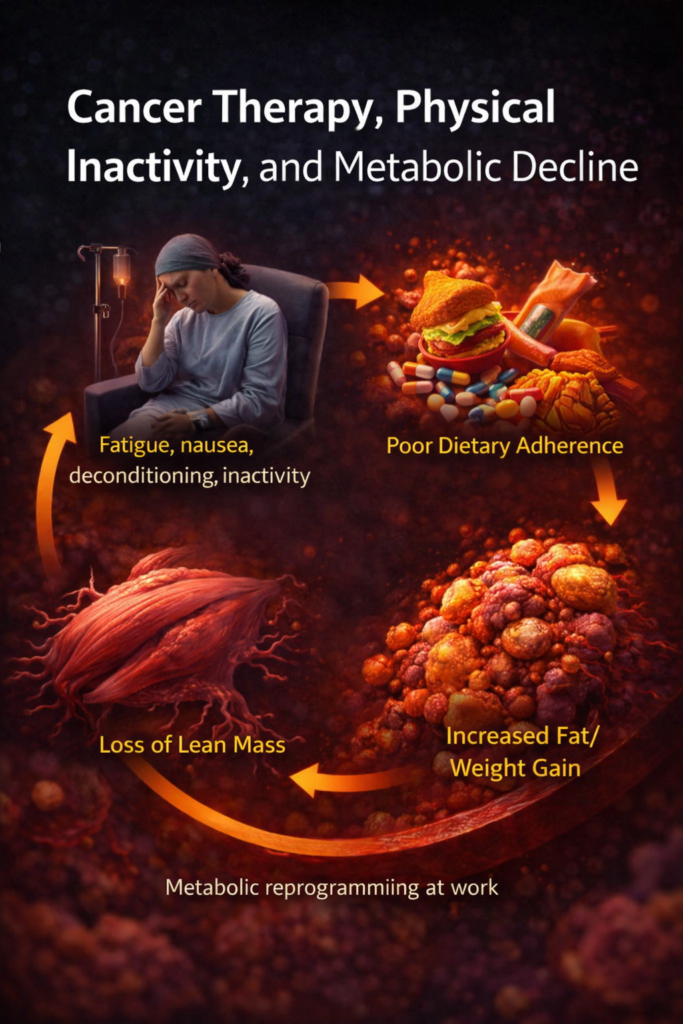
Cancer treatment often brings fatigue, nausea, deconditioning, and reduced physical activity. Dietary adherence suffers. Lean muscle mass declines. Adiposity increases. Weight gain becomes common.
These changes compound pre-existing cardiometabolic risk and accelerate progression of dyslipidemia and atherosclerotic disease. Without intentional intervention, cardiovascular vulnerability quietly worsens during a time when patients are least equipped to recognize it.
What Should Be Done—And Why It Matters

Lifestyle modification remains foundational and should be actively reinforced throughout cancer treatment. Patients should be encouraged—within their limits—to remain physically active, maintain dietary quality, and avoid unnecessary discontinuation of preventive therapies.
When indicated, statins should be initiated or continued during cancer treatment. Importantly, lipid goals for patients undergoing cancer therapy or for cancer survivors are no different from those of the general population and should follow standard cardiovascular risk–based guidelines.
Drug–drug interactions deserve attention. Several statins are metabolized via the cytochrome P450 system, raising concerns when used alongside systemic cancer therapies. In such cases, alternative agents such as pravastatin may offer a safer option.
Evidence That Cardiovascular Prevention Works in Cancer Care
The strongest randomized evidence supporting statin use in cardio-oncology comes from the STOP-CA trial. In this study, patients with lymphoma received atorvastatin 40 mg daily starting before anthracycline therapy and continuing for 12 months. The result was a significant reduction in anthracycline-associated cardiomyopathy, with the greatest benefit seen in higher-risk patients—older individuals and those receiving higher cumulative anthracycline doses (3).
For trastuzumab-associated cardiotoxicity, emerging data from meta-analyses and observational studies suggest a lower incidence of cardiac events among patients treated with statins, though randomized trials remain limited. Similarly, observational evidence indicates reduced major adverse cardiovascular events following radiation therapy in patients receiving statins—again highlighting promise in an area still awaiting definitive trials.
The Takeaway
Cardiovascular disease does not wait for cancer treatment to end.
Dyslipidemia and other cardiovascular risk factors are common, modifiable, and too often neglected in patients with cancer. Maintaining guideline-directed cardiovascular care during cancer treatment is not optional—it is essential. The goal is simple but powerful: allow patients to survive cancer without sacrificing their cardiovascular future.
References
- Calip G.S., Boudreau D.M., Loggers E.T. Changes in adherence to statins and subsequent lipid profiles during and following breast cancer treatment. Breast Cancer Res Treat. 2013;138(1):225–233.
- Calip G.S., Elmore J.G., Boudreau D.M. Characteristics associated with nonadherence to medications for hypertension, diabetes, and dyslipidemia among breast cancer survivors. Breast Cancer Res Treat. 2017;161(1):161–172.
- Neilan T.G., et al. Atorvastatin for Anthracycline-Associated Cardiac Dysfunction: The STOP-CA Randomized Clinical Trial. JAMA. 2023;330(6):528–536. doi:10.1001/jama.2023.11887.
— Anusha Bhat, MD, MPH
Cardio-Oncology | Cardiovascular DiseaseYour Attractive Heading
